Table of Content
Blog Summary:
This guide explains everything about health insurance software development, starting with the basics. To help you understand better, we discuss its importance, types, benefits, applications, innovations, future trends, and much more. Keep reading to grasp more.
Table of Content
Health insurance is one of the fastest-growing businesses. A recent report by Research and Markets suggests that the US healthcare insurance market will be approximately USD 1.59 trillion in 2025 and reach USD 2.13 trillion by 2030. In this booming industry, insurers need to cater to the needs of a growing number of customers seeking smart health solutions.
Due to the increasing number of customers, insurers often face challenges maintaining transparency, efficiency, and personalized services. Opting for health insurance software development is the right solution.
A powerful health insurance software lets insurers serve customers with recommendations for the right plan, appropriate medical assistance, and treatments. A fully functional, feature-driven, and robust app gives them a competitive edge by allowing them to grab opportunities to serve more customers.
However, developing a full-fledged health insurance app involves extensive planning. To make your task easier, we have provided a complete guide to health insurance software development.
Health insurance software is an application that automates and streamlines operations within this industry. It includes unmatched potential to improve accuracy, efficiency, and customer satisfaction by managing vital processes in a fully centralized platform.
Developing healthcare software solutions contributes greatly to policy-making. Insurers can use them to perform various tasks like customization, designating, and managing health insurance plans quite conveniently. They bring automation to the claiming process while ensuring fast approvals, timely reimbursements, and accurate validations.
Health insurance software is a specialized digital solution that streamlines and automates various operations within the health insurance industry. Its core purpose is to enhance efficiency, accuracy, and customer satisfaction by managing critical processes in a centralized platform.
When it comes to integrated billing features, it ensures smooth invoicing, premium management, payment tracking, and more. It also supports customer service by providing fully secure portals for clients. Clients can access the portals to check, file claims, and receive assistance.
With these capabilities, health insurance software improves productivity, minimizes manual errors, and thus ensures full compliance with regulatory standards. It also plays an indispensable role in redefining the entire insurance operation by making it more advanced and efficient. It improves everyone’s experience, whether they are policyholders or service providers.
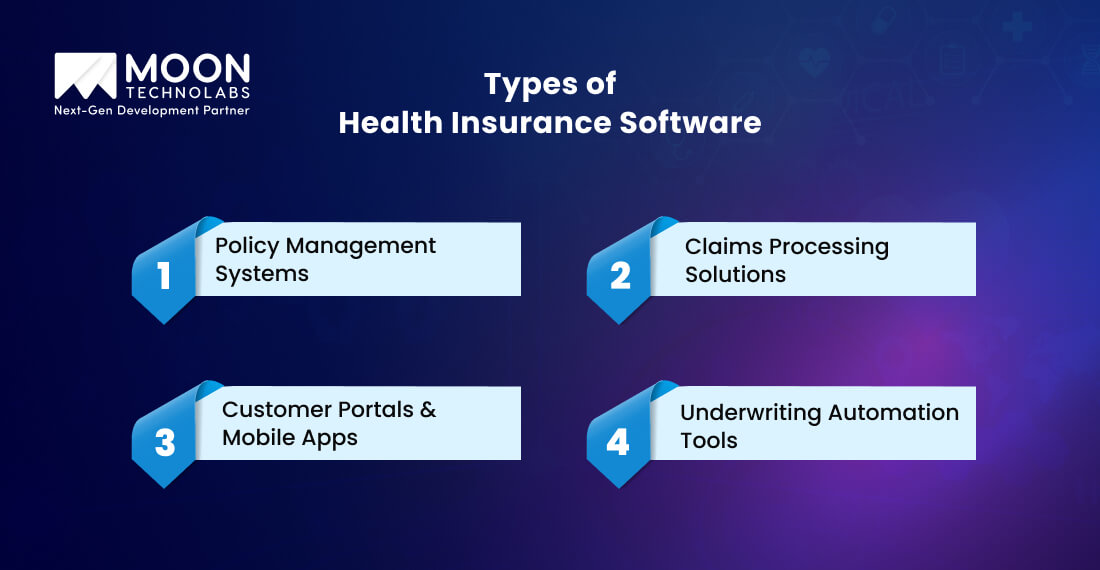
Different types of healthcare insurance software serve different purposes, such as transforming operations or improving customer experience. We cover some of the most important types of software that health insurers leverage most frequently:
Policy management systems are useful for insurers for various purposes, including policy creation, renewals, updates, and cancellations. They can automate policy documentation, monitor changes, and offer complete centralized access to policy information for both customers and insurers.
A claim processing solution is important to simplify and speed up the entire claiming process, from submission to settlement. It checks eligibility, determines coverage, automates payment processes, and thus detects fraud. Advanced solutions leverage Machine Learning (ML) and AI for risk assessment and flag discrepancies. They minimize both human error and processing time.
With these tools, policyholders have the flexibility to gather insurance details. The site boasts a myriad of features, such as submitting claims, viewing coverage, accessing support, making payments, and more.
The software improves the user experience by offering telemedicine options, real-time notifications, document uploads, and more. It boosts transparency and engagement.
Underwriting software can automate the risk evaluation process for new policies. It gathers data from different sources, such as credit reports, medical records, past claim history, and more. It leverages rule-based algorithms to improve the speed and accuracy of underwriting decisions.
Health insurance software development is important to match the emerging needs and expectations of customers. Let’s explore some other reasons:
Health insurance software is important to ensure full compliance with healthcare regulations like GDPR, HIPAA, and more. These systems are also important for managing and protecting personal and sensitive health. They include advanced encryption and access control features.
The software automates many compliance tasks and securely stores data, minimizing the risk of data breaches and legal penalties. It’s also effective in creating trust and reliability with clients.
Manual processes often require more time and are also highly prone to errors. Health insurance software can tackle these things efficiently. It automates the entire workflow and thus ensures quick decision-making while minimizing operational costs.
The software facilitates smooth data integration between third-party systems and different departments. With a higher operational efficiency, insurers can manage a larger volume of clients.
Insurers can meet customers’ expectations by offering convenient, fast, and personalized services. Health insurance software facilitates insurers’ provision of mobile applications and user-friendly apps where customers find it convenient to see complete policy details, track progress, submit claims, get support, etc.
Features such as automated reminders and AI-driven chatbots let policyholders engage and get informed. By enhancing responsiveness and transparency, insurance providers can increase loyalty and satisfaction.
Check out how we have developed a similar AI-powered app to track policies and process claims, InsurNow.
Investment in customized healthcare software helps modernize legacy systems. Although initially expensive, this minimizes long-term expenses. Automating many repetitive tasks also reduces labor costs. Meanwhile, real-time analytics is useful for preventing fraud and optimizing pricing strategies.
Efficiency claims handling effectively minimizes overall payout errors and accelerates reimbursements. Insurance companies can boost their profitability by minimizing waste and thus increasing overall service delivery.

As we already mentioned, healthcare insurance software improves operations and thus overall efficiency. We cover some other advantages of leveraging health insurance software for insurers:
Since manual processing is error-prone and time-consuming, dedicated insurance software automates the entire process. The automated process is less prone to errors and thus speeds up the entire process. Automated workflows let policyholders get on-time reimbursements, which indeed boosts customer satisfaction.
Whether it’s data analytics or AI, these technologies are perfectly integrated into insurance software that analyzes lifestyle choices and individual health data to recommend tailored insurance policies.
Personalization plays a vital role in improving user engagement. It allows insurance companies to provide relevant products, which improve both customer retention and conversion rates.
Another major feature of advanced health insurance software is its powerful data analytics abilities. Insurers have wonderful opportunities to access real-time dashboards that offer complete insight into claims trends, risk assessment, customer behavior, and operational performance. Data-driven decisions allow organizations to optimize offerings and thus minimize potential losses.
Fraudulent claims are an important concern in the insurance industry. Robust health insurance software implements technologies like AI and ML algorithms to discover anomalies and thus reflect suspicious activities. The software lets insurers prevent fraud while saving both financial resources and time.
A perfect and smooth integration of the hospital system with Electronic Medical Records (EMRs) is essential for a holistic healthcare experience. Health insurance software ensures hassle-free data exchange between insurers and service providers. It also ensures quick claim processing, accurate billing, and enhanced patient care coordination.
Improve accuracy and efficiency in your healthcare insurance process with our advanced app solutions tailored to match your healthcare business.
Healthcare insurance software is useful for different segments for a range of purposes. We cover some of the major usages of this software in detail:
Insurance agencies and brokers benefit greatly from leveraging this software. It automates everything, be it claims processing, policy management, or customer engagement.
The software facilitates insurers in making easy comparisons of different plans and quick onboarding, thus improving customer service. Brokers leverage software to personalize offerings and thus boost client retention.
Third-party administrators play an intermediary role between insured parties and insurers. Health insurance software eases complications in claims adjudication, compliance tracking, network management, and more.
TPAs can automate various processes, such as monitoring claim fraud and approvals, and maintaining a detailed record. This speeds up the claim settlement process and improves cost control.
Welfare initiatives and public health schemes utilize custom health insurance platforms for managing enrollment, larger-scale data, policy tracking, and subsidy distribution. Automation’s major advantage is that it ensures higher transparency, minimizes administrative burdens, and analyzes healthcare provider performance and eligibility. It also provides real-time analytics for public health planning and policy making.
Corporate offerings of group healthcare insurance to their staff leverage customized software to track claims, monitor utilization, manage enrollment, and more. When the software is integrated with the HR system, it offers smooth updates to employee data.
It also provides self-service portals that encourage staff to access their policy details to raise claims, thus improving their workplace satisfaction.
With advanced health insurance software, policyholders can easily approach healthcare service providers from any location. It ensures preventive care and easy access to healthcare and thus minimizes overall hospitalization costs.
Insurers can gain an advantage from minimized claim volume and improved customer engagement. Integrating wellness platforms into software solutions also allows them to track everything, be it diet, goals, or chronic diseases, using apps or wearables.
Software development for health insurance witnessed a massive transformation due to the emergence of several technologies. Here, we discuss some of the technologies that contribute to shaping the future of this software:
AI has transformed customer support in the health insurance sector. AI-driven chatbots help policyholders with status tracking, real-time claim filing, document submission, and more.
These virtual assistants can minimize wait times, function 24/7, and handle even larger numbers of queries with greater accuracy, preventing your staff from handling complex tasks.
Blockchain is a powerful technology that facilitates medical records sharing among providers, patients, and insurers by maintaining transparency and security. Its immutable ledger minimizes any risk of fraud or data breaches.
It also ensures smooth data access across many authorized parties. This kind of innovation builds trust, speeds up claim approvals, and enhances underwriting accuracy.
Predictive analytics is useful for forecasting future health risks and medical costs. It harnesses the power of ML and big data to predict with higher accuracy. Insurers can analyze lifestyle factors, historical data, claims trends, etc.
These help them identify many high-risk patients early. It ensures preventive interventions, which minimize the overall long-term healthcare expenses.
Insurers can integrate IoT devices with healthcare solutions, such as smartwatches or fitness trackers, into insurance platforms to analyze policyholders’ health metrics. These metrics include heart rate, activity levels, and sleep quality.
Insurers utilize real-time data to reward healthy behavior with wellness incentives or premium discounts. This offers healthy lifestyles while minimizing claims.
Voice-based systems leverage technologies, including natural language processing (NLP). They have become an important part of call centers and health insurance apps. Users can easily interact with these systems to get coverage clarifications, check policy details, file claims hands-free, etc. These tools can improve accessibility for the visually impaired.

Many factors are responsible for evolving future trends in health insurance software development, whether it is frequently changing customer expectations or technology advancements. We explain some of the future trends.
Most insurers have recently been leveraging technologies like data analytics and AI, especially with increasing access to personal health data through EHRs and wearable devices. They use these technologies to personalize insurance plans.
They tailor plans based on factors such as lifestyle, health profile, risk factors, and more. This ensures higher customer satisfaction and accuracy in pricing models.
InsurTech is a result of emerging decentralized finance (DeFi) and Blockchain technologies. InsurTech 3.0 platforms offer smart contracts, peer-to-peer models, and higher transparency. They minimize fraud, administrative overhead, claim processing time, and more. Thus, they provide result-driven insurance ecosystems.
AI has transformed underwriting through the automation of data collection and risk assessment. It facilitates insurers in determining underwriting policies and claims processes quickly and with improved accuracy. It boosts operational efficiency while minimizing human errors and biases.
Nowadays, most customers expect convenience and accessibility. Mobile-first design has become crucial for many policyholders, who submit claims, manage policies, access customer support, and more through mobile apps and self-service portals. These solutions minimize users’ dependency on call centers and thus streamline their service delivery.
No or low-code platforms gained vast popularity among insurers because they speed up the software development process. These tools allow them to create, test, and implement insurance apps even with less coding expertise.
So, the democratization of software development minimizes the overall innovation cycles and ensures fast responses based on market demands.
Many healthcare giants have already developed healthcare software and integrated it into their existing systems to unlock its numerous benefits. Their projects reflect the role of innovation in improving patient experience, efficiency, and minimizing costs across different healthcare ecosystems. We discuss some of the top projects:
Problem
Oscar Health came across many challenges in managing member engagement and offering timely and personalized customer service. Their existing systems could not match their unique needs, which caused huge inefficiencies in communication.
Solution
The company created a custom CRM platform capable of offering a centralized dashboard. It allowed customer service teams to track communication histories, manage member interactions, and offer proactive messaging. It integrated perfectly with Oscar’s benefits and claims and many provider networks to provide a smooth experience.
Outcome
The final solutions ensured huge satisfaction among members. They also positively impacted retention by offering real-time and personalized support, making customer service more efficient and faster.
Problem
Aetna’s old and traditional claiming process was slow, causing inaccuracies and higher operational costs. This prompted the company to build a solution that could help them overcome such problems.
Solution
The company developed solutions by incorporating an AI-driven engine that used ML algorithms to automate the claim review process. The system could predict approval probabilities, analyze claims data, and detect anomalies.
Outcome
The newly developed system minimizes manual errors and turnaround times and speeds up provider payment. It can also detect inconsistencies and fraud and boost operational efficiency.
Problem
UnitedHealth required a system that could identify at-risk individuals early for the prevention of costly health complications, chronic disease progression, hospital readmission, and more.
Solutions
It has built a predictive analytics platform that can analyze different data sources, including lifestyle factors, patient records, social determinants of health, etc. The platform leverages ML and big data to predict many potential health risks.
Outcome
The predictive platforms helped the company by offering on-time interventions and care management programs, boosting patient outcomes, and minimizing hospital readmissions.
Problem
Cigna faced issues with its healthcare services, such as benefits, claims, and provider networks. The systems faced huge inefficiencies and also delayed information sharing between stakeholders.
Solution
Cigna built healthcare solutions with an API-first strategy. This allowed smooth data exchange between its internal systems, pharmacies, providers, and various third-party platforms. It also standardized data sharding and provided real-time benefit verification, care coordination, and eligibility checks.
Outcome
The final solution improved Cigna’s operational efficiency. It also improved workflow and patient experience through secure and fast data exchange.
Moon Technolabs specializes in developing healthcare insurance software to help businesses flourish. We work with the core commitment to shape the features of health insurance software development.
We possess vast technical expertise to create custom health insurance software that matches your unique challenges of health insurance. Our developers are familiar with customer expectations, regulatory requirements, and security needs. Based on these, we create high-end software that aligns perfectly with your business goals.
We understand that every business has a unique need. It prompts us to build tailor-made solutions to match your specific business goals. Whether you require management software, policy, claim processing tools, or customer engagement systems, we create solutions that boost operational efficiency while minimizing operational costs.
We understand the importance of healthcare data security. Our developers take a security-first approach to each project to ensure that the software incorporates the latest industry standards. We safeguard your sensitive data by implementing powerful security measures. We are committed to protecting your business by minimizing the risk of data breaches and penalties.
We are proficient in integrating with your existing systems while ensuring the free flow of data across various platforms. Whether you wish to integrate with CRM platforms, EHRs, or third-party apps, we perform multiple tasks to build deserving solutions for your business.
We are concerned not only about developing healthcare insurance software but also about ensuring its smooth functionality for a long time. With us, you get ongoing support and maintenance services to ensure the smooth functionality of your software. Whether it’s troubleshooting, timely updates, or enhancements, our services include everything.
We create healthcare insurance apps developed to match your specific and core business requirements. Opt for our solutions to redefine your business operations.
Health insurance software development has redefined the way providers, insurers, and customers communicate. This technology has enormous capabilities, from automating the claiming process to improving user experience.
Moreover, technologies including IoT, Blockchain, and AI make the future of this software more promising with personalized solutions. Contacting Moon Technolabs helps you build robust, scalable, and secure software.
01
02
03
04
05
Submitting the form below will ensure a prompt response from us.