Table of Content
Blog Summary:
AI is here to completely revamp the medical billing process through task automation, error reduction, and efficiency improvements. This blog explores how AI strengthens billing processes, its benefits, top software solutions, challenges, and best practices for implementation. Additionally, we’ll discuss the future of AI in medical billing and its capability to modernize healthcare financial operations.
Table of Content
Healthcare is evolving, and so is medical billing. Digital records and practice management software have paved the way, but AI is taking things to a whole new level. This isn’t just about automation. It’s about intelligent solutions that can dramatically improve accuracy and efficiency. Curious about how AI can streamline your medical billing?
This blog will walk you through the key aspects of AI in Medical Billing, from understanding its mechanics to mastering its implementation. Let’s discover the medical billing ecosystem through the world of artificial intelligence.
AI is revolutionizing medical coding primarily by utilizing machine learning and natural language processing. AI systems help to accurately analyze patient records, including complex clinical notes, and assign the correct billing codes.
This automation minimizes the risk of human error, which is a major cause of claim denials and revenue loss. Furthermore, AI ensures that coding practices adhere to the latest industry standards, reducing the likelihood of compliance issues.
Beyond coding, AI is simplifying the entire claims processing workflow. Manual claims processing is notoriously time-consuming and prone to errors. AI automates the verification of patient data, diagnosis codes, and payer-specific rules. Hence, there are now faster and more accurate claim submissions.
This results in quicker reimbursements, improved cash flow, and reduced administrative overhead for healthcare organizations. Moreover, AI’s ability to detect inconsistencies and potential errors in real time significantly reduces the number of denied claims.
Another very important use case of AI is its ability to detect fraud. AI algorithms analyze large amounts of data and find patterns that indicate fraudulent activity.
In addition to these core functions, AI is improving the patient experience by automating billing and providing real-time insurance verification. AI-powered systems generate accurate patient bills, taking into account insurance coverage and individual payment plans.
This transparency improves patient satisfaction and reduces billing-related inquiries. Furthermore, instant insurance verification helps to prevent unexpected out-of-pocket expenses and ensures that patients receive the appropriate care based on their coverage.
Ultimately, AI is optimizing the entire revenue cycle, enabling healthcare providers to focus more on delivering quality patient care.
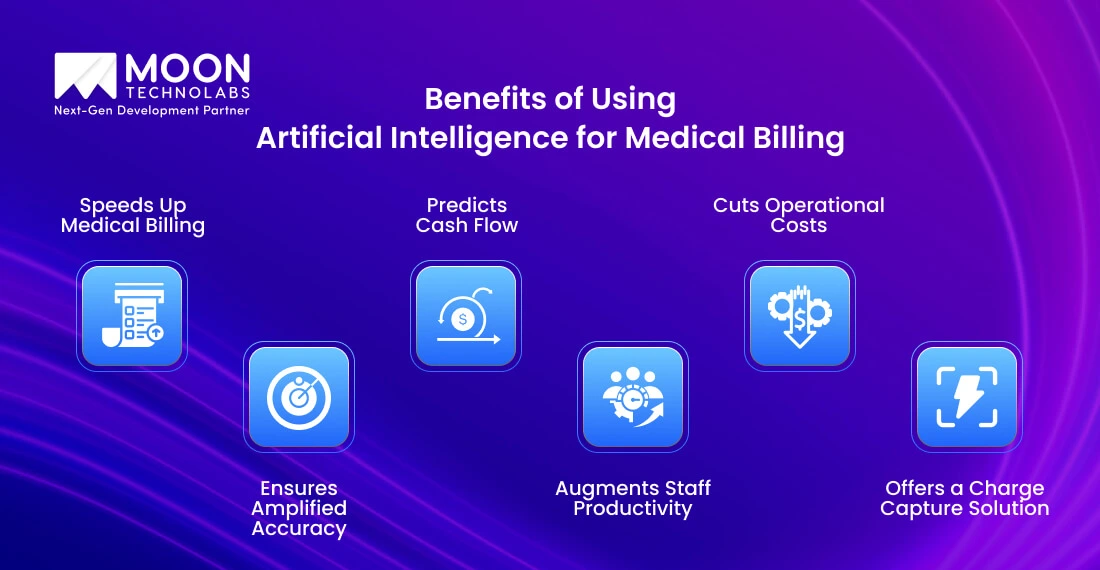
AI boosts medical billing and coding through faster processing, greater data capacity, and superior accuracy, minimizing human error. Let’s check out the main advantages:
AI automates billing processes. Hence, manual effort is reduced, and faster claim submissions are ensured, allowing healthcare providers to scale without increasing administrative workload.
AI minimizes human errors in coding and documentation. As a result, it leads to lesser claim denials and faster reimbursements.
AI helps analyze billing data to forecast revenue. Hence, healthcare providers can easily manage their finances and plan better.
AI takes over repetitive billing tasks, allowing staff to focus on more complex responsibilities and improving overall efficiency.
Automating billing reduces labor costs and addresses staff shortages by performing tasks that would otherwise require additional personnel.
AI ensures that all services are accurately documented and billed, preventing revenue loss due to missed charges.
You Might Also Like:

Now, let’s discover how AI automates tasks, improves accuracy, and streamlines the medical billing workflow for more efficient healthcare management.
AI automatically extracts and inputs patient information from various sources, such as electronic health records (EHRs), insurance cards, and scanned documents. It helps reduce manual data entry errors and streamline patient registration and management processes.
Additionally, AI helps automate appointment scheduling and reminders to improve patient flow.
Medical coding is complex, involving assigning standardized codes to diagnoses and procedures. AI, particularly through natural language processing (NLP), analyzes patient records and clinical notes to assign these codes accurately.
This minimizes coding errors, which are a major cause of claim denials. AI then uses these codes to generate accurate and compliant insurance claims automatically.
AI systems verify claims in real time against payer rules and regulations, spotting potential errors before submission. This prevents claim denials and minimizes the need for expensive modifications. By identifying errors before submission, the time it takes for a medical office to receive reimbursement is shortened.
Machine learning algorithms have the power to analyze payment patterns and identify potential frauds. AI can also automate payment posting and reconciliation, ensuring that payments are accurately recorded and applied. AI can also be used to create better predictions of when payments will be received, improving financial forecasting.
AI can analyze vast amounts of billing data to identify trends and patterns, such as common claim denials, underpayments, or areas for revenue optimization. This provides valuable insights for healthcare providers to improve billing practices and revenue cycle management. AI also assists in tracking key performance indicators and providing reports to management.
Now, let’s explore the best medical billing software solutions designed to streamline revenue cycles for healthcare providers.
Kareo Billing is designed to help independent practices manage their billing processes. It offers features for claims management, patient billing, and reporting and is known for its user-friendly interfaces. It is geared towards smaller independent practices.
AdvancedMD provides a comprehensive suite of solutions, including medical billing, EHR, and practice management. It offers robust claims management with features like automated claim scrubbing. Additionally, it has strong reporting and analytics capabilities and is a more comprehensive system that can handle larger practices.
DrChrono is a mobile-first platform that offers EHR and medical billing solutions. It is known for its user-friendly interface and mobile accessibility. It provides features for claims management, patient billing, and e-prescribing. Moreover, DrChrono is popular with smaller practices that want mobile flexibility.
AthenaCollector is a cloud-based revenue cycle management solution that automates billing processes and reduces claim denials. Athenahealth provides a very comprehensive solution and is a strong option for larger medical groups.
AI has revolutionized medical billing, but it’s not without its hurdles. From data privacy concerns to integration issues with legacy systems, various challenges hinder seamless adoption. Additionally, inaccuracies in coding, compliance risks, and the need for human oversight highlight AI’s limitations in this complex field. Let’s explore these obstacles in detail.
Medical billing is governed by constantly evolving regulations, such as HIPAA in the U.S. or GDPR in Europe. AI models must continuously adapt to changes in coding practices (ICD, CPT) and compliance laws. Failure to stay updated leads to claim rejections, financial losses, or legal issues.
AI’s effectiveness depends on high-quality, standardized data. However, medical records often contain errors, missing information, or inconsistencies across healthcare providers. Variations in EHR (Electronic Health Record) formats and interoperability issues can limit AI’s ability to process claims accurately.
AI must balance efficiency with ethical considerations like patient confidentiality, data privacy, and unbiased decision-making. If AI systems make billing errors, patients may be overcharged, leading to financial and legal disputes. Additionally, liability issues arise when AI-driven decisions negatively impact patient care.
Healthcare professionals and billing staff may hesitate to adopt AI-driven systems due to concerns over job security, reliability, and trust in automated processes. Many organizations prefer traditional methods, fearing potential errors, high implementation costs, and the need for extensive training.
Don’t worry—you have the best experts in the industry. We’ll handle the entire medical billing process for you.
Now that we are well-versed in the pros and cons, let’s discuss the best practices for using AI in medical billing.
You can deploy AI throughout the workflow to overcome claims processing challenges. This approach delivers improved accuracy and efficiency. It also addresses key issues by automating patient data entry, capturing charge details, streamlining submissions, correcting errors, and optimizing denials.
AI offers significant capabilities, but it also necessitates human oversight. Regular audits following installation are crucial for upholding accuracy, ensuring compliance, and maximizing performance.
AI-powered automation significantly reduces manual workload, freeing up your team. To maximize its effectiveness, maintain active oversight and collaborate closely with your software provider. Together, you can map the AI’s capabilities to your specific workflows and ensure seamless integration.
Predictive analytics empowers you to optimize both patient care and financial performance. By analyzing data, you can anticipate revenue trends and develop personalized treatment plans.
AI tools provide the transparency needed to refine your revenue cycle and identify critical patterns in patient data. This strategic approach transforms data into actionable insights, leading to improved patient outcomes and increased revenue predictability.
Claims issues arise from a multitude of causes. AI empowers you to pinpoint specific problems, such as procedural weaknesses and human errors. By analyzing these patterns, you can optimize your revenue cycle and minimize claim rejections. Furthermore, AI provides the insight needed to address systemic root causes, leading to lasting improvements.
Medical billing is about to change because AI and automation are combining to make it more accurate, faster, and patient-focused. Here’s a breakdown of how AI is shaping the future of this critical healthcare function:
AI is streamlining repetitive tasks like data entry, claim submission, and payment processing, reducing human error and accelerating workflows.
AI algorithms analyze historical data to forecast payment trends, identify potential delays, and optimize revenue cycles. This allows healthcare providers to address issues and improve financial stability proactively.
AI can detect anomalies and patterns in billing data that may indicate fraudulent activity, helping to prevent financial losses and ensure compliance.
AI-powered patient portals can provide real-time updates on billing status, personalized payment plans, and clear explanations of charges, enhancing patient satisfaction and trust.
AI helps identify areas for improvement in billing processes, such as reducing claim denials and optimizing coding practices. This leads to increased revenue and reduced costs.
AI systems can continuously learn from data and adapt to changing regulations and billing practices, ensuring ongoing accuracy and efficiency.
AI is being integrated with electronic health records (EHRs) and other healthcare technologies, enabling seamless data exchange and streamlining workflows.
By automating tasks, reducing errors, and optimizing revenue cycles, AI is helping to lower administrative costs and improve the overall efficiency of healthcare operations.
Automate and optimize your billing workflow with AI. Our team will ensure a seamless and successful implementation.
Moon Technolabs streamlines your medical billing with over a decade of expertise in healthcare app development solutions. We empower healthcare organizations, from solo practitioners to large facilities, with technology-driven processes and multi-layered quality assurance.
Our proactive approach to regulatory changes and our commitment to timely submissions ensure a seamless billing cycle. Contact us now to discover how we can transform your medical billing.
Artificial intelligence offers healthcare organizations significant solutions through automated billing, revenue forecasting, and fraud detection. This leads to improved efficiency and sustainability. However, adopting AI presents challenges.
Moreover, safeguarding patient data privacy and security is paramount, and seamlessly integrating AI with existing systems can be complex. Implementation costs and staff training requirements pose hurdles, especially for resource-constrained practices.
In that case, it’s best to partner with specialized service providers like Moon Technolabs, who will help you navigate these complexities.
01
02
03
04
Submitting the form below will ensure a prompt response from us.